The Clock is Ticking: End Tuberculosis, An Existing Microbial Threat
WHAT IS TUBERCULOSIS?
Tuberculosis (TB) is an airborne bacterial infection caused by Mycobacterium tuberculosis (M. tuberculosis) (Figure 1.) that usually affects the lungs (known as pulmonary TB)1,2. TB can spread through the inhalation of respiratory droplets of an infected person1,3. TB is a severe condition that can be fatal if not appropriately treated1.

Depending on the airflow in the environment, the respiratory droplets can remain suspended in the air for several hours unless removed by natural or mechanical ventilation4. Therefore, daily disinfection of surfaces with mycobactericidal agents is required, particularly in hospitals and clinics4.
Did you know there are two types of pulmonary TB infections3?
In most people who inhale M. tuberculosis, the body’s natural immune system can fight the TB infection3. As a result, not everyone infected with TB will become ill3. For those who cannot fight-off TB infection, there are two TB-related conditions that exist3:
- Active TB – Active TB infection refers to when the infection has overcome the body’s immune system, multiplied, and spread to other parts of the body, causing symptoms3,5.
- Latent TB – Latent TB infection refers to someone who is infected with M. tuberculosis but does not present with active TB symptoms and does not feel ill3,5. Latent TB can develop into active TB in people whose immune systems have been weakened over their lifetime or due to medical conditions5. Refer to table 1 for a comparison of the two TB-related conditions.
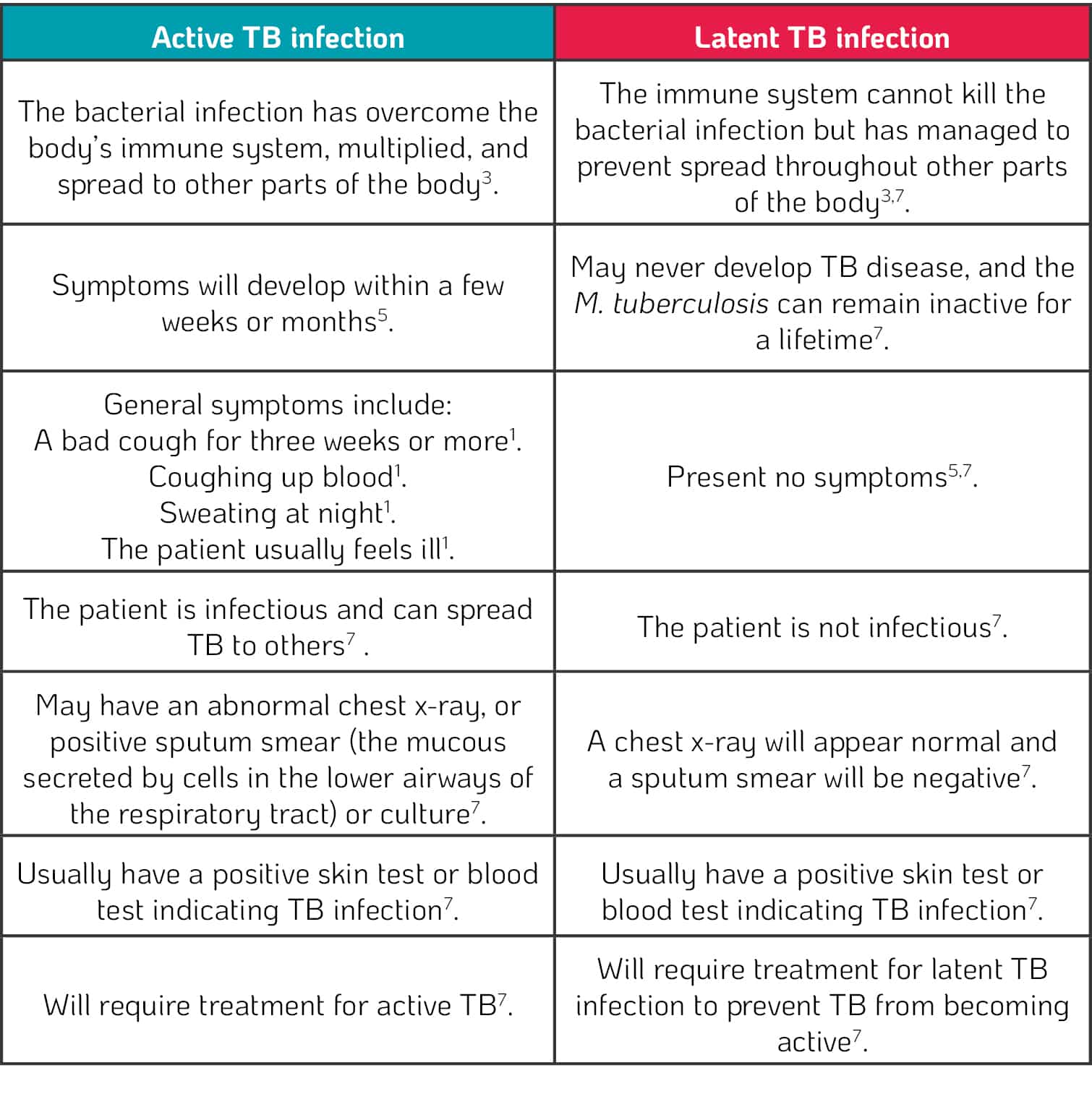
Table 1. Comparison of active and latent TB infections
Did you know TB can also develop in other parts of the body5?
It is possible for TB infections to develop in areas outside the lungs (extrapulmonary TB)5, such as in the lymph nodes, the bones and joints, the digestive system, the bladder, the reproductive system, and the nervous system4. Usually, TB infections in other parts of the body are not infectious6 and are more common in people who have a weakened immune system5.
WHO IS AT RISK?
All age groups and ethnicities are at risk of TB1. However, there are risk factors that increase the likelihood of contracting TB including:
• Working or residing with people at high risk for TB in facilities such as hospitals, nursing homes and homeless shelters8.
• Underlying medical conditions in young children and immunocompromised individuals such as human immunodeficiency virus (HIV) and diabetes mellitus8.
• Misusing alcohol and smoking tobacco8.
• Recovering from active TB infection8.
• Residing in crowded conditions8.
• Residing in or visiting an area with high levels of TB8.
WHAT ARE THE MOST COMMON SYMPTOMS OF TB?
Did you know for active TB, the symptoms may be mild for many months leading to delays in seeking medical advice1,5? – This increases the probability of transmission to others1.
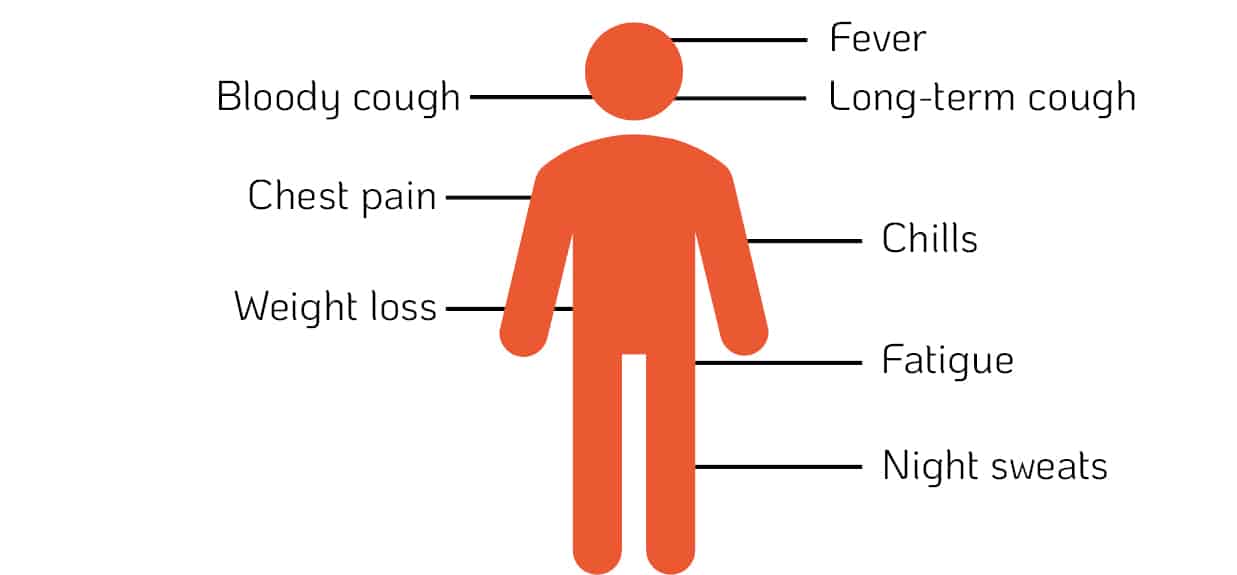
Common Symptoms of Active Pulmonary TB 1,3,7
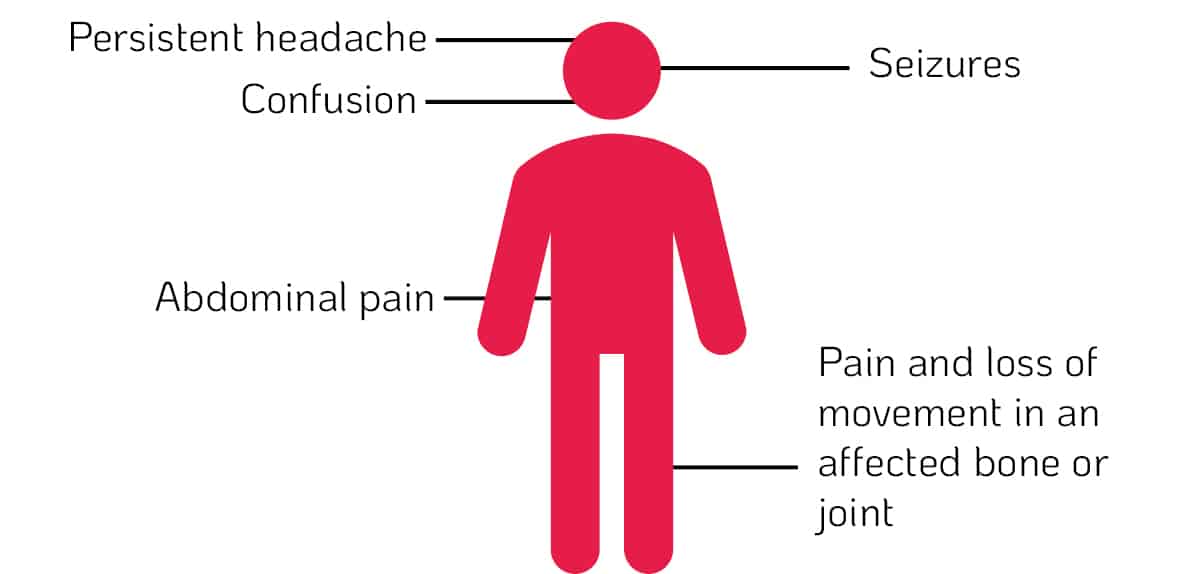
Common Symptoms of Extrapulmonary TB5
WHY IS TB A MICROBIAL THREAT?
Did you know the COVID-19 pandemic could potentially cause an additional 6.3 million TB cases worldwide by 20259?
The COVID-19 pandemic may reverse all progress made in ending TB9. The implementation of social distancing measures may help reduce TB transmission9. However, this could be offset by longer durations of infectiousness; increased likelihood of exposure to TB infection within the household; worsening outcomes due to a decrease in care-seeking behaviour of the infected and the extra pressure on health services; and higher levels of poverty, particularly among the most vulnerable populations where severe economic contractions and loss of income occurs9. COVID-19 has placed significant financial pressure on the availability of global funding commitments from governments for the TB response9. Several countries with resources initially allocated for TB have diverted the funds to the COVID-19 response for their citizens9. The combination of TB and COVID-19 effects on a person’s respiratory and immune system could prove to be deadly.
Did you know only two in three people with drug-resistant TB have access to treatment10?
Multidrug-resistant TB (MDR-TB) has emerged as a global health crisis11. MDR-TB is the consequence of anti-TB medicine misuse, incorrect prescription, low-quality drugs, and patients prematurely stopping treatment1. MDR-TB patients will not respond to isoniazid and rifampicin, the two most potent first-line anti-TB drugs10. In this case, second-line TB drugs will be used to treat MDR-TB1. However, extensively drug-resistant TB (XDR-TB) has also emerged globally, where TB patients do not respond to the most effective second-line anti-TB drugs1. Although XDR-TB is challenging to treat, it is not impossible10. A third more severe drug resistance, known as totally drug-resistant TB (TDR-TB), has also developed, often leaving patients without further treatment options10.
Did you know TB is the leading killer of people with HIV8?
TB co-infection with HIV can be a lethal combination to an infected individual1. People living with HIV are eighteen times more likely to develop active TB1. HIV weakens the immune system enabling the TB infection to thrive in the body1. On average, without proper treatment, about 45% of HIV-negative people with TB will die1. In comparison, nearly all HIV-positive people with TB will die1. People living with HIV are now dying because of TB, despite the advancements made to improve their quality-of-life1.
THE CLOCK IS TICKING
Everyone is susceptible to TB9. People with TB can be found in every country and from all age groups1. Areas with the highest TB cases include India, Indonesia, China, the Philippines, Nigeria, Pakistan, Bangladesh, and South Africa1,3. It is estimated 4000 lives are lost daily, 12,000 lives lost monthly, and 1.5 million lost yearly due to TB12.
Did you know about a quarter of people worldwide are infected with M. tuberculosis and are at risk of developing active TB1,8?
It is time to act by testing and treating latent and active TB infections13. It is time to speak up and eliminate the stigma associated with TB that may prevent people from seeking medical care13. This can be done by improving public education and awareness of TB13. The hope of having a world free of TB, leading to zero deaths, disease and suffering because of TB, is achievable. However, everyone will have a part to play in preventing the spread of TB worldwide.
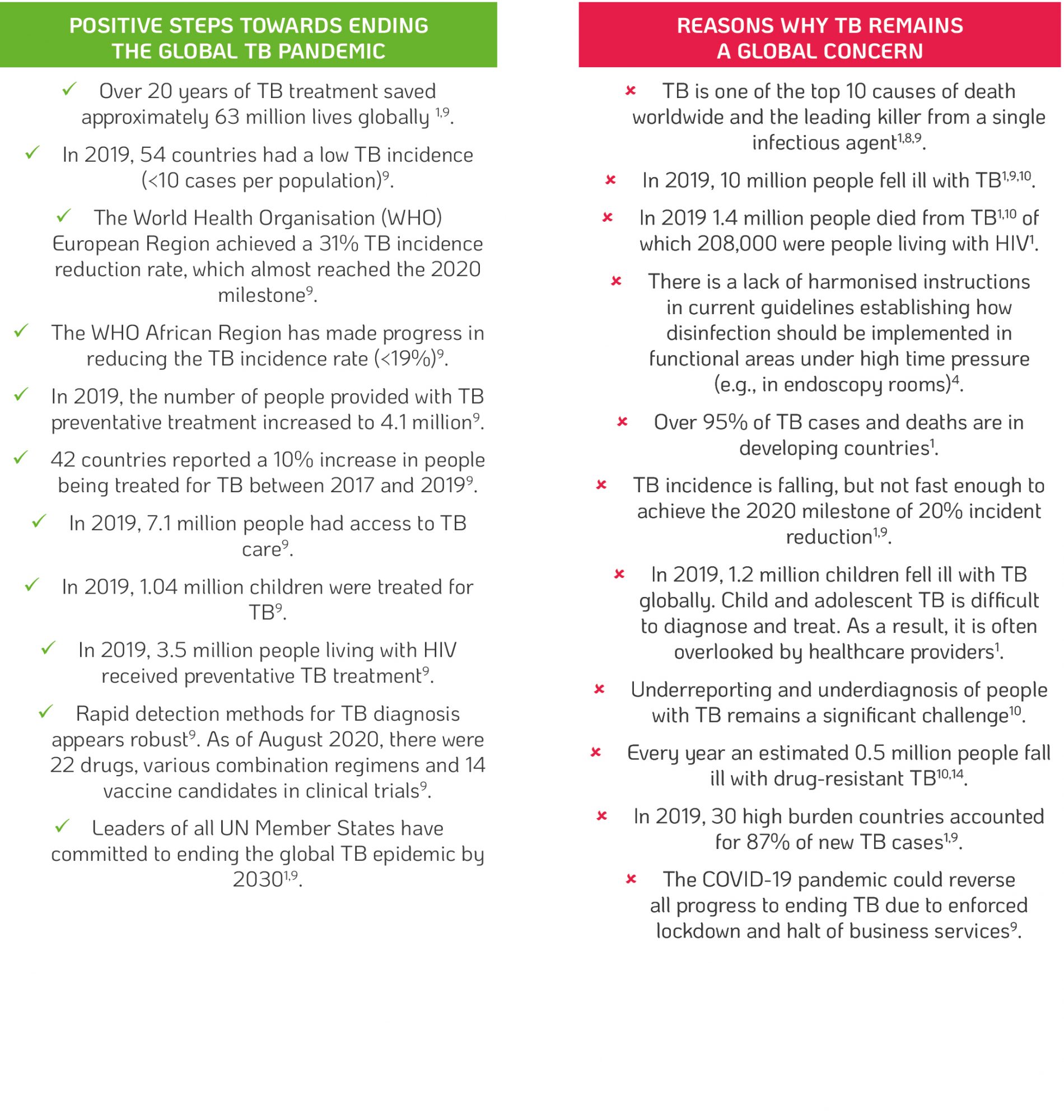
Table 2. Highlighting positive steps towards eradicating TB and reasons why TB remains a global concern.
PROPRIETIES OF M. TUBERCULOSIS
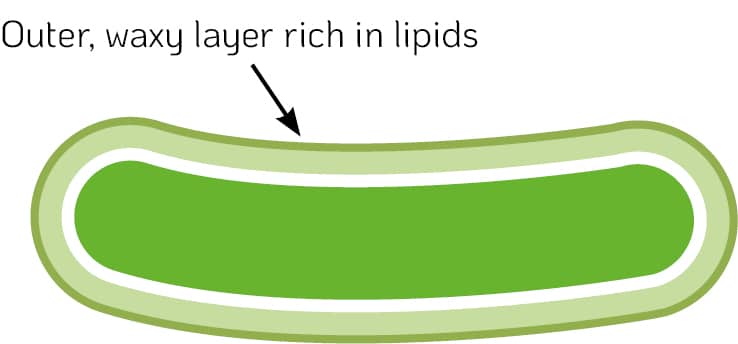
Mycobacteria species have a unique cell wall and outer membrane composition, which includes: a thick peptidoglycan layer, lipopolysaccharides, embedded glycolipids, wax esters and mycolic acids (long fatty acids chains) that lend to the mycobacterial impermeable barrier17,18. The mycobacterial cell wall characteristics (Figure 2.) facilitate:
1. Survival in different environments, including biofilms, soils, and water17,18.
2. Resistance to disinfection procedures as the waxy outer envelope can prevent disinfectant entry to the mycobacterial cell17,18.
Did you know surfaces and medical devices can be a continuous source of transmission for pathogens such as M. tuberculosis if no regular preventative disinfection is performed?
M. tuberculosis can persist on surfaces for up to four months19. High-touch surfaces such as door handles, railings, chairs, and table tops may be potential transmission sources. Medical devices that make direct contact with the respiratory system, such as laryngoscopes, bronchoscopes, nasopharyngoscopes, gastrointestinal (GI) manometry catheters and transoesophageal probes, could all be carriers of M. tuberculosis.
Figure 2. M. tuberculosis waxy cell envelope
AVAILABLE DIAGNOSIS AND TREATMENT
Diagnosis of TB for many countries is assessed by sputum (a mixture of saliva and mucous coughed up from the respiratory tract) smear microscopy15. This detection method involves trained laboratory technicians examining sputum samples under a microscope to determine if TB mycobacteria are present. However, this method detects only half the number of TB cases and cannot detect TB drug resistance15.
Rapid molecular diagnostic tests have high diagnostic accuracy and are recommended by the WHO for anyone with signs and symptoms of TB, as the initial diagnostic test1. The rapid tests lead to significant improvements in the early detection of TB and MDR-TB1. Xpert MTB/RIF, Xpert Ultra, and Truenat assays are the rapid tests recommended by the WHO1. TB treatment typically involves the use of multiple
medicines in a variety of combinations16. The combination will depend on the individual’s circumstances. A first time TB infection will be treated differently from a reoccurring TB infection, and if a residential area is known to have antibiotic resistance to any TB drug treatment16. Active, drug-susceptible TB is a treatable and curable disease1. Typically, adherence to a standard six-month3 course of four antimicrobial drugs and support for the patient by a healthcare worker or trained volunteer successfully facilitates recovery9. However, treatment adherence can be problematic for people with limited access to TB treatment facilities9,16. Those who have active MDR-TB contribute to the difficulty healthcare professionals have in successfully treating TB9,16.
PREVENTION AND INFECTION CONTROL MEASURES
Health care interventions available to reduce the risk of TB include:
• Adherence to infection prevention – maintaining good hand hygiene and conducting disinfection of medical devices and surfaces that can be carriers of TB4.
• Preventative TB treatment for latent TB infection7.
• Implementing a global multisectoral approach on determinants such as poverty, housing quality and undernutrition to tackle TB9.
• Encouraging the reduction in the prevalence of health-related risk factors for TB such as smoking, alcohol misuse, diabetes, and HIV infection, which
can help decrease the number of TB related cases worldwide1.
• BCG vaccination protects from severe TB in children, especially in countries with a high TB-burden and in households with people living with HIV3.
Did you know people infected with TB can infect up to 15 other people through close contact over a year1?
If you have been diagnosed with TB, please follow your doctor’s advice to limit the spread. Such advice may include:
• Ensure to take prescribed TB treatment as ineffective treatment can lead to transmission and antibiotic resistance3.
• Ensure to cover the mouth with a tissue when coughing or sneezing and dispose of tissues carefully in a sealed bag3.
• Ensure to wash hands regularly3.
• Ensure to avoid large crowd gathering and public transportation3.
• Do not return to work, school or college until the specialist has confirmed you are no longer infectious3.
TRISTEL EFFICACY
Prevent the spread of TB and other pathogens by:
• Ensuring the surfaces in the vicinity of patients and staff are disinfected.
• Ensuring the device is high-level disinfected after each patient use.
Quaternary ammonium compounds (QACs) are less effective against mycobacteria, especially in the presence of protein residues, i.e., soiling.
QACs work by disrupting the cell wall, leading to the cytoplasm leaking out of the cell21. QACs mode of action is limited by the mycobacteria’s waxy outer cell walls21 (Figure 2.). This is because QAC active components are hindered from causing cell wall disruption to deactivate/destroy mycobacteria21. QACs are considered low or intermediate level disinfectants and may require long contact times to achieve the required efficacy level. A surface or device must remain visibly wet for the recommended product contact time during the disinfection process, or reapplication is required. This can be difficult to achieve, especially in the medical environment, where time constraints are critical to reducing patient waiting times and increasing patient turnaround. QACs are not recommended as high-level disinfectants due to their poor efficacy against mycobacteria and spores22.
Tristel’s high-level disinfecting chlorine dioxide-based products, offer a full spectrum of microbial efficacy including against mycobacterium species. Tristel chlorine dioxide-based products are mycobactericidal following the required European Norm (EN) test standards stipulated in EN 14885:2018. Tristel products including Tristel Fuse for Stella (for use with Stella), the Tristel Trio Wipes System and Tristel Jet GEL for Surfaces have been tested and are proven effective against Mycobacterium terrae and Mycobacterium avium. M. terrae is the surrogate species for M. tuberculosis, and as a result, it is acceptable for a product to claim tuberculocidal efficacy [against TB] when possessing this data. Efficacy against both Mycobacterium species, M. terrae and M. avium, enables a product to be termed ‘mycobactericidal,’ inferring efficacy against all Mycobacterium species.
USE TRISTEL CHLORINE DIOXIDE PRODUCTS TO PROTECT YOUR DEVICES AND SURFACES

STELLAQuick, mobile, and economic reprocessing of single-lumened and non-lumened, heat-sensitive medical devices. |

TRISTEL TRIO WIPES SYSTEMA comprehensive solution for the decontamination of semi-critical, non-lumened medical devices. |

Tristel JETA sporicidal disinfectant foam, ideal for use on high-touch surfaces. |
For references see PDF download. ©2021 Tristel Solution Limited. All rights reserved.