Candidozyma auris (formerly known as Candida auris) is a rapidly emerging pathogenic yeast. Individuals who have recently stayed in nursing homes and have lines and tubes that go into their body (such as breathing tubes, feeding tubes and central venous catheters) seem to be at the highest risk for C. auris infection. Spanning five continents, Candidozyma auris has been responsible for prolonged outbreaks in countries such as India, Pakistan, Venezuela, Colombia, Spain, Israel, South Africa, and the USA.
What do I cause?
If C. auris enters the bloodstream and spreads throughout the body, it can cause invasive candidiasis (an infection caused by the yeast Candida spp.).
C. auris has caused bloodstream infections (Candidemia), wound infections, and ear infections.
Why am I a microbial threat?
C. auris infections have been reported from over 30 countries and are often multidrug-resistant and resistant to multiple antifungals commonly used to treat yeast infections. Only a few antifungal types exist, so resistance can severely limit treatment options. Some strains are resistant to all available classes of antifungals.
Did you know? The prevalence of C. auris infection is unknown and likely underreported due to misidentifying C. auris as other yeasts or bacteria, making detecting and controlling this pathogen difficult.
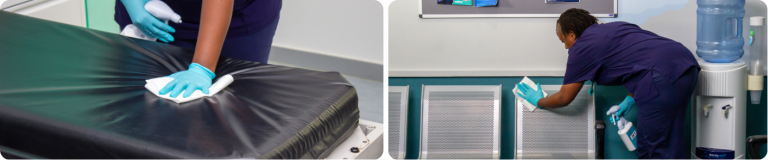
Where can I be found?
C. auris as a particular preference for skin, particularly moist areas like the armpit and groin. During the recent podcast, Candidozyma auris from the lab to the front line: A discussion with UKHSA experts, specialists highlighted that the daily shedding of millions of human skin cells facilitates the easy transfer of C. auris between individuals and to surfaces.
According to the UKHSA’s Candidozyma auris (formerly Candida auris): guidance for acute healthcare settings (GOV.UK), environmental contamination of C. auris is extensive, and survival times of seven days have been recorded on general surfaces, increasing to four weeks for some plastic devices.
Studies have identified that C. auris may be present throughout patient environments, extending beyond patient rooms to hallways. Specific high-touch surfaces and medical equipment found to be contaminated include:
- Beds
- Chairs
- Window sills
- Sinks
- Taps
- Floors
- Doors
- Counters
and devices like:
- Stethoscopes
- Electrocardiogram leads
- Blood pressure cuffs
- Infusion pumps
- Ventilators
C. auris has the potential to colonise hosts within days to weeks of exposure. Colonisation with C. auris may persist for many months and possibly indefinitely, and from a colonised state, invasive infections can develop within days to months.
Did you know?
C. auris was first isolated from the external ear canal of a patient in Japan in 2009.
How am I transmitted?
C. auris has caused outbreaks in healthcare settings. It can spread through contact with contaminated environmental surfaces or equipment or from person to person.
It is essential to identify asymptomatic colonised patients to take additional precautions when placing indwelling devices or surgical intervention. These patients may also be a source of transmission to other patients and environmental contamination.
Did you know? C. auris can survive on moist and dry surfaces for at least 14 days.
How can you defend against me?
The best practice is to use a high-level disinfectant that incorporates robust, broad-spectrum biocidal chemistry that can be expected to destroy bacterial spores, fungal spores, vegetative bacteria, mycobacteria, yeast, and viruses.
Notably, the UKHSA specifically cautions against using quaternary ammonium compounds (QACs) due to insufficient evidence of efficacy against C. auris. Furthermore, hydrogen peroxide vapour and ultraviolet light systems should only be considered as supplementary measures and not substitutes for full cleaning and disinfection protocols.
Disinfectants known to be effective against Clostridioides difficile spores, including chlorine dioxide and peracetic acid, are generally considered effective against C. auris.
Did you know? High-level disinfectants will prevent the spread of harmful pathogens from one patient to another while safeguarding healthcare professionals during routine procedures.