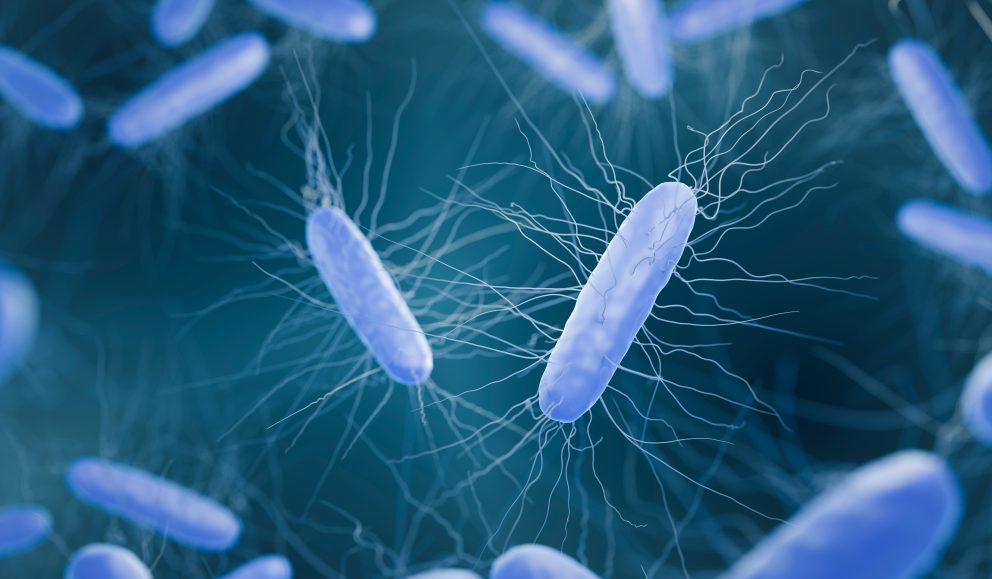
Clostridioides difficile, formerly known as Clostridium difficile, is a spore-forming bacterium that causes mild to severe diarrhoea and intestinal conditions like colitis (colon inflammation).
Where Can I Be Found?
C. difficile usually live harmlessly in the bowels; therefore, the bacteria and their spores can be found in faeces.
C. difficile colonisation, defined as the detection of the organism without symptoms, is common, occurring in:
- 15%–30% of residents in long-term care facilities
- 4%–15% of healthy adults
- Up to 21% of hospitalised adults
Did you know?
C. difficile is the most frequent cause of infectious diarrhoea in hospitals and long-term care facilities.
What Do I Cause?
For healthy people, C. Difficile does not pose a health risk. However, sometimes when antibiotics are taken, the balance of bowel microbial flora can change. This reduction in microbial diversity allows C. difficile to multiply and produce toxins. These toxins can damage the bowel and cause diarrhoea.
Most cases of C. difficile infection occur while taking antibiotics or not long after the course is finished. The severity of illness can vary, from mild diarrhoea to serious conditions such as pseudomembranous colitis, bowel perforation, sepsis, and in extreme cases, even death.


Why Am I a Microbial Threat?
C. difficile can affect anyone, but certain environments and risk factors increase the likelihood of infection. In healthcare settings, where many patients are receiving antibiotics, the presence of C. difficile can lead to frequent outbreaks. The risk of infection is higher for individuals who:
- Have had a previous C. difficile infection
- Have recently stayed in a hospital or nursing home
- Are aged 65 or older
- Have weakened immune system, such as those with HIV/AIDS, cancer, or organ transplant patients taking immunosuppressive drugs.
These factors make C. difficile a significant microbial threat, particularly in vulnerable populations.
Did you know?
About 1 in 6 patients who get C. difficile will likely get it again in the following 2-8 weeks.
How Am I Transmitted?
People can get infected if they touch surfaces contaminated with faeces and then touch their mouths. Healthcare workers can spread the bacteria to their patients if their hands are contaminated.
How Can You Defend Against Me?
To help prevent the spread of C. difficile infections, always wash your hands with soap and water after using the bathroom and always before eating.
Use a separate bathroom, take showers and wash with soap if possible. Wash clothes and sheets contaminated with faeces separately from other washing at the highest possible temperature. Clean the toilets, commodes, and the area around them with disinfectant after each use.
Did you know?
C. difficile can survive on surfaces for up to 5 months because they resist the bactericidal effects of most hospital disinfectants and other decontamination techniques.
Disinfectants with Sporicidal activity are essential for infection control and defence against C. difficile. The best practice is to use a high-level disinfectant incorporating robust, broad-spectrum biocidal chemistry to destroy small numbers of bacterial spores, most fungal spores, all common vegetive bacteria, mycobacteria, yeast, and viruses.
Emerging Strain: C. difficile RT955
A newly evolving strain of C. difficile RT955 has emerged in areas of the UK, posing fresh challenges for infection control. This strain has proven more difficult to cultivate under standard testing conditions, making it harder to evaluate using traditional methods.
We’re proud to share new test data demonstrating the efficacy of our high-level disinfectant, JET LUX, against C. difficile RT955:
| Product | Test | Conditions | Log Reduction |
|---|---|---|---|
| JET LUX | EN 17126 Suspension test | Clean | 3.80 |
| JET LUX | EN 17126 Suspension test | Dirty | 4.01 |
Did you know?
High-level disinfectants will prevent the spread of harmful pathogens from one patient to another while safeguarding healthcare professionals during routine procedures.
Meet our Surface Solutions
References:
Centres for Disease Control and Prevention, National Centre for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP) (2022). What Is C. diff? [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/cdiff/what-is.html.
Claro, T., Daniels, S. and Humphreys, H. (2014). Detecting Clostridium difficile Spores from Inanimate Surfaces of the Hospital Environment: Which Method Is Best? Journal of Clinical Microbiology, [online] 52(9), pp.3426–3428. doi: https://doi.org/10.1128/jcm.01011-14.
GOV.UK (2022). Clostridioides difficile: guidance, data, and analysis. [online] GOV.UK. Available at: https://www.gov.uk/government/collections/clostridium-difficile-guidance-data-and-analysis.
HSE (2023). Clostridioides difficile. [online] HSE.ie. Available at: https://www.hse.ie/eng/services/list/2/gp/antibiotic-prescribing/conditions-and-treatments/gastro/clostridium-difficile/.
NHS (2022). Clostridium difficile. [online] NHS. Available at: https://www.nhs.uk/conditions/c-difficile/.
Public (2014). Fact Sheet – Clostridium difficile (C. difficile) – Canada.ca. [online] Canada.ca. Available at: https://www.canada.ca/en/public-health/services/infectious-diseases/fact-sheet-clostridium-difficile-difficile.html.